As much as I hate to admit it, at times I feel like Sisyphus, pushing the boulder up the hill only to have it roll down the other side, only to have to push it back up the hill and roll down again, over and over and over again for all eternity. Certainly trying to keep track of pseudoscience in medicine and trying to educate why so much of so-called “complementary and alternative medicine” (CAM) is quackery (and the stuff that isn’t quackery is just medicine rebranded as CAM) and why “integrative medicine” involves integrating quackery with medicine can seem like a very Sisyphean task. I was reminded of this by a press release from the National Center for Complementary and Integrative Health (NCCIH) right before Thanksgiving that I had meant to write about before a couple of topics popped up that interested me more. Besides, the infiltration of alternative medicine quackery into medicine in the form of CAM and integrative medicine or health is ongoing, and the paper touted by NCCIH is just more evidence:
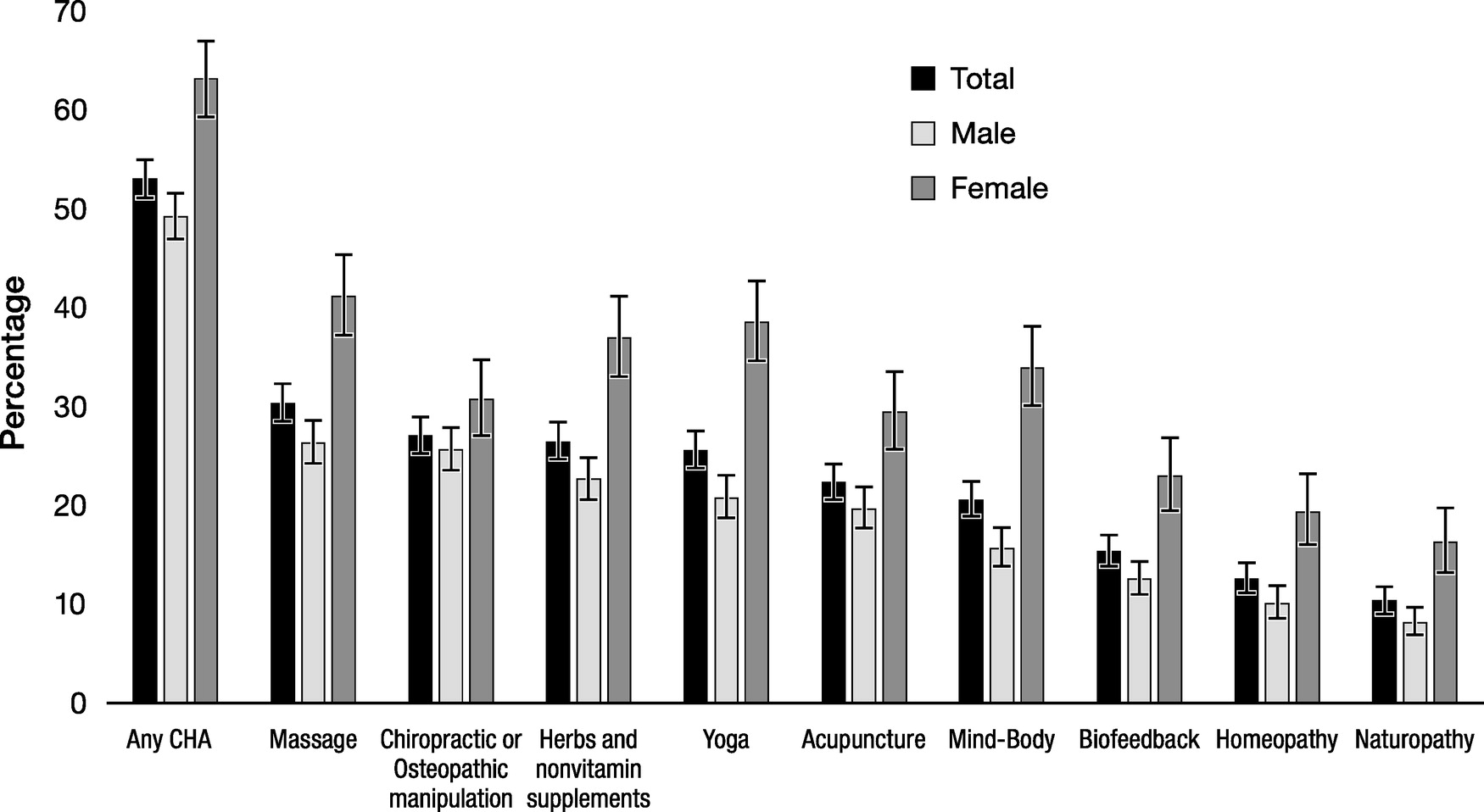
More than half of office-based physicians recommend at least one complementary health approach to their patients, according to a new analysis of data from a nationally representative survey. In addition, female physicians recommended every complementary health approach at a higher rate than male physicians except for chiropractic and osteopathic manipulation. The analysis was conducted by researchers from the National Center for Complementary and Integrative Health (NCCIH) and the National Center for Health Statistics (NCHS), and was published in The Journal of Alternative and Complementary Medicine.
Here’s the study. It is, as mentioned above, the product of researchers at NCCIH. In the introduction, the authors make an assertion that I find very startling:
Complementary and integrative health practices, interventions, and natural products include mind–body interventions such as massage therapy, acupuncture, and yoga, and natural products such as fish oil or probiotics,1 and are widely used by U.S. adults.2,3 Despite data on use of complementary health approaches (CHAs) by adults,3–6 there are no nationally representative data using a probability sample collected on the recommendations for CHAs by U.S. office-based physicians. Studies in this area have been limited to certain medical specialties (e.g., rheumatology, pediatrics, and family practice),7–14 U.S. regions,15–17 or types of CHAs (e.g., mind–body therapies and chiropractic).8,18,19 These have found recommendation rates by physicians for different CHAs were relatively high. For example, a national survey of rheumatologists found a majority were likely to recommend body work (65%), meditation (64%), and acupuncture (54%) for chronic lower back and joint pain,7 67% of pediatricians in a Seattle hospital reported recommending CHAs to patients,15 more than half of physicians in the Chesapeake area referred patients to practitioners of biofeedback and chiropractic,20 and 25% of physicians from the Hawaii Medical Service Association had/would refer patients for CHAs.16
What I found startling is that there aren’t a lot more data on the recommendation patterns for CAM over more specialties and over the whole country. After all, what has it been that NCCIH has been doing the last 25+ years? I especially wonder why, given that the figures that are published for CAM usage and recommendations are always used by advocates for an appeal to popularity, to represent CAM as being very popular and therefore worthy of study and, by implication, use. Of course, to do that, CAM advocates have to include a fair number of modalities as “CAM” that really aren’t, such as prayer, vitamins, exercise modalities (tai chi, qi gong, and yoga), and the like. This survey of doctors is no different.
So how did the investigators go about estimating what percentage of office-based physicians who recommend CAM modalities, which, for whatever reason, the authors decided to call “complementary health approaches” (CHA)? Basically, they mined the 2012 Physician Induction Interview of the National Ambulatory Medical Care Survey (NAMCS PII), a nationally representative survey of office-based physicians. The NAMCS website reveals that it’s a program of the Census Bureau. The Census Bureau describes the program thusly:
The National Ambulatory Medical Care Survey (NAMCS) is the Nation’s foremost study of ambulatory care provided at physicians’ offices and has been conducted since 1973. It focuses on visits made to non-federally employed, office-based physicians who are primarily engaged in direct patient care. Since 2006, the survey also includes an annual sample of visits to community health centers (CHCs). From 2012 through 2015, a new sampling design allowed NAMCS to make estimates not only for the nation and four Census regions, but also for up to as many as 34 of the nation’s most populous states. NAMCS provides information on patient, provider, and visit characteristics. It is sponsored by the Centers for Disease Control and Prevention’s (CDCs) National Center for Health Statistics (NCHS), and is administered by the U.S. Census Bureau.
So, the NAMCS appears to be a robust data source on the practices of office-based physicians all over the country. Here’s how it’s administered:
Each year, the National Center for Health Statistics (NCHS) scientifically selects a random group of physicians and CHCs throughout the country to participate in NAMCS. This group of physicians is selected from a list of licensed non-federal physicians in office-based practice maintained by the American Medical Association and the American Osteopathic Association. These lists are continually updated by both associations to make them as current and accurate as possible at the time of sample selection. The list of CHCs selected for participation comes from the Health Resources and Services Administration (HRSA). If you are selected, you will receive a letter in the mail from NCHS informing you of that before the Census Bureau contacts you.
Here’s where you can find some of the data produced by the NAMCS, along with some publications that resulted from its data, and here are some of the survey instruments.
Here’s how the NCCIH investigators used the NAMCS:
For the “any CHA” category, a “yes” response to the question was included, “During the past 12 months, did you recommend any of the following therapies or practices to your patients?” Therapies asked included massage therapy, herbs/other nonvitamin supplements, chiropractic/osteopathic manipulation, yoga, acupuncture, mind–body therapies (i.e., guided imagery, meditation, and progressive muscle relaxation, not including prayer), naturopathic treatment, biofeedback/hypnosis, and homeopathic treatment. Based on the literature, demographic characteristics included in the analysis were physician age, sex, race, and medical specialty (general/family practice, internal medicine, psychiatry, obstetrics/gynecology, pediatrics, and all other specialties combined), type of physician (doctor of medicine [MD] or doctor of osteopathic medicine [DO]), medical school location (United States or foreign), metropolitan statistical area (MSA)/non-MSA, and U.S. Census region (Northeast, Midwest, South, and West).7–11,15,23,24 Ethnicity was not included as there were not enough Hispanic respondents to produce reliable statistics. Because several therapies had small cell sizes prohibiting subgroup analyses, the majority of analyses were restricted to the six most prevalent individual therapies (i.e., massage therapy, herbs/nonvitamin supplements, chiropractic/osteopathic manipulation, yoga, acupuncture, and mind–body therapies), but included all nine in the “any CHA” category. To avoid small cell sizes and present statistically reliable estimates, physician’s age was collapsed into 4 categories (<45, 45–54, 55–64, and ≥65 years), race into 3 categories (white, Asian, and other), and 12 physician specialties (general surgery, orthopedic surgery, cardiovascular diseases, dermatology, urology, neurology, ophthalmology, otolaryngology, oncologists, allergists, pulmonologist, and other specialties) into 1 “other specialty” category.
There are two figures summarizing the results:
These results are truly depressing. Over 50% of physicians have recommended a CHA in the last year. Of course, these numbers are inflated, as they are with all such surveys, by the inclusion of a modality like massage. Massage is a perfect example of what I like to refer to as a patient support service that’s become medicalized. Massage, when properly done, feels good, and that should be enough for its use. There’s also nothing “complementary” or “integrative” about it. If massage can be used to relieve pain or loosen joints, it’s part of medicine.
I’m also not surprised that chiropractic or osteopathic manipulation was recommended by 27% of physicians. Sadly, chiropractors have been so successful at representing their specialty as a legitimate medical practice that too many doctors view it as basically interchangeable with physical therapy when, as I like to say, chiropractors are incompetent physical therapists with delusions of grandeur. While physical manipulation can indeed alleviate back pain, for instance, chiropractors claim to be able to treat systemic diseases such as asthma, allergies, diabetes, and more. They’re also very antivaccine, and their manipulation of the neck has real risks. Here’s a word of advice to my colleagues: Don’t ever refer to a chiropractor. Refer patients who might benefit from manipulation or exercise to physical therapy or occupational therapy instead of a chiropractor or an osteopath.
What really depresses me is not so much how many physicians had recommended massage or chiropractic in the 12 months before they were surveyed. Nor does it bother me as much that over one quarter of physicians had recommended vitamins, supplements, or yoga. Yes, it does bother me that so many physicians recommend vitamins and supplements without good evidence for their efficacy in anything, but it bothers me more how many physicians recommended acupuncture (22.4%), homeopathy (12.6%), and naturopathy (10.4%). I’m sorry, but if you can’t understand that homeopathy is The One Quackery To Rule Them All, with tenets underlying it that violate the laws of physics and chemistry and that would, if true, require rewriting those laws, then you should not be a physician, period. Similarly, if you don’t understand that naturopathy is a hodgepodge of pseudoscience and quackery mixed with some sensible interventions based on diet and lifestyle (although, truth be told, even the science-based interventions used by naturopaths are usually tainted with pseudoscience), you should not be a physician. As Harriet Hall has so aptly put it, what’s good about naturopathy (emphasis on healthy diet and lifestyle) is not unique to naturopathy, and what’s unique to naturopathy (quackery like homeopathy) is not good.
This survey does, however, reemphasize what I’ve been saying all along about acupuncture, as being the “gateway” quackery that lets in a lot of other stuff behind it. Many years ago, I once thought there might be something to acupuncture. The more I read, the more I studied it, though, the more I realized that it’s just a theatrical placebo and that its only effects are nonspecific placebo effects. However, unlike the case for homeopathy, where it’s pretty easy to explain why it’s nonsense, an explanation that frequently leaves medical students and fellow physicians to whom I relate it shaking their heads because they had always assumed that homeopathy was just herbal medicine, acupuncture involves actually sticking needles into the body. A lot of physicians therefore assume that there must be something to it. Sure, those who know enough about it will concede that the concepts of meridians and unblocking the flow of qi are ridiculous, but then they’ll cite claims by acupuncturists and researchers who believe in acupuncture about “releasing endorphins” or other biological mechanisms claimed for its efficacy. They don’t know about the retconned history of traditional Chinese medicine and acupuncture, its basis in astrology and bloodletting, or that the filiform needles now used in acupuncture were only introduced 80 years ago. Add to that the way advocates spin negative acupuncture studies as being positive, and I can see how physicians who don’t pay as close attention as we do to the literature might think there’s something to it, and it doesn’t help how successful acupuncturists have been in obtaining the imprimatur of the state by persuading state legislatures to license their “profession.”
The study also shows what specialties tend to recommend more CHAs. Disappointingly, at the top of the heap were general and family practice doctors, 75.5% of whom had recommended a CHA, 52.6% of whom had recommended chiropractic, and 36.1% of whom had recommended acupuncture in the last year. Internal medicine doctors weren’t much better, recommending the same CHAs at a rate of 64.8%, 39.9%, and 28.7%, respectively, with psychiatrists following close behind at a rate of 62.7%, 12.4%, and 27.7%, respectively. (I guess it’s not surprising that psychiatrists would have less call to recommend chiropractic, given the conditions they treat.) Other specialties (general surgery, orthopedic surgery, cardiovascular diseases, dermatology, urology, neurology, ophthalmology, otolaryngology, oncology, allergy, pulmonology, and other specialties) were the least likely to recommend CHAs at a rate of 29.9%, 16.3%, and 16.1%, respectively.
Table 2 in the paper and the supplemental tables, break down the rates of recommendation of CHA by a variety of factors. For example, female physicians were more likely to recommend CHAs than males (49.3% verus 63.2%, adjusted odds ratio 1.56), as were DOs (aOR 1.78), who were, unsurprisingly, also a lot more likely to recommend chiropractic or osteopathic manipulation. Oddly enough, there wasn’t an age effect on the likelihood of a physician to recommend a CHA. The aORs ranged from 0.93 to 1.23, and all the 95% confidence intervals spanned 1.0. There were differences in likelihood to recommend specific CHAs by age of physician (physicians 65 and older were less likely to recommend yoga and massage therapy, for instance), but not overall for a recommendation of any of the CHAs examined. I would have predicted that younger physicians might be more open to CAM than older physicians, and that prediction was clearly wrong. The rates of CAM recommendation are roughly equal over all the physician age cohorts examined, although the authors made it sound as though this were not the case in the discussion by citing other studies finding younger doctors to be more open to CAM. Finally, there were regional differences, with doctors in the Northeast, Midwest, and South census regions (particularly the South and Midwest; the difference was not as great for the Northeast) significantly less likely to recommend CHAs than those in the West, which intuitively does not seem surprising.
The authors conclude:
The current findings add to the literature by showing physician-based national estimates regarding sex differences in recommendations of CHA. Female physicians recommended CHAs at a higher rate than male physicians (63.2% vs. 49.3%, respectively), with this difference remaining even when controlling for additional characteristics. Furthermore, female physicians were approximately twice as likely to recommend each individual therapy, except chiropractic/osteopathic manipulation. These findings confirm and expand upon prior studies that found female physicians more likely to talk to patients about CHAs9 or recommend CHAs.8 Likely related to female physician recommendations is the fact previous studies have consistently found higher usage rates of CHAs among U.S. women than among men,5,6 and likewise found physicians who report personal usage of CHAs more likely to recommend CHAs to patients.8,15 Furthermore, previous research has found that U.S. health care workers, and, in particular, health care providers, are more likely to use CHAs than workers in other occupations.38 Given the rising rate of female physicians in the United States,39 there is reason to expect that recommendations for CHAs will increase over time.
I have seen the data that more females use CAM than males, but I just wonder if that’s a function of increased health care utilization by females in general compared to males. It is, however, rather disappointing to learn that health care workers are more likely to use CAM than the general public.
Finally:
This study analyses show that physicians often recommend CHAs, with 53.1% of office-based U.S. physicians recommending at least one to their patients in the past 12 months. Recommendation rates were higher among female physicians than among male physicians and varied by medical specialty. General/family practitioners and internists recommended CHAs at higher rates than pediatricians, and more than half of psychiatrists recommended mind–body therapies, compared with <30% of physicians from other specialties. Understanding practice patterns of U.S. physicians related to recommendations for CHAs, and their differences across medical specialties and physician sex, could inform consumers, physicians, and medical schools.
My question is: Inform them of what? How many doctors recommend quackery to their patients in addition to medicine? In reality, this study is very much like every other NCCIH study examining CAM usage: Its function is marketing, not “to inform”. Expect it to be used to argue how popular CAM is, how many doctors accept it, and thus to argue to policymakers and insurance companies that CAM should be reimbursable by government and private health insurance plans.